When More Actually IS Better
By: Julie Bartels and Mike Stoecklein
At the ThedaCare Center for Healthcare Value, we see our mission as transformation of the healthcare system to assure the delivery of consistent, high quality care, and better outcomes for patients. 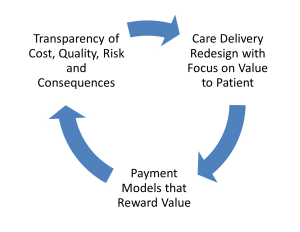 We envision achieving this transformation in collaboration with patients and leaders in the provider, employer, insurer, and government communities. Together, we can create a one-piece flow of value as depicted by the diagram on the right. But it requires involvement on several different fronts.
We envision achieving this transformation in collaboration with patients and leaders in the provider, employer, insurer, and government communities. Together, we can create a one-piece flow of value as depicted by the diagram on the right. But it requires involvement on several different fronts.
One way that we support this work is through peer-to-peer learning networks. At present, we have two such interdependent networks. The Healthcare Value Network (HVN) is primarily focused on the upper right-hand part of the diagram, “Care Delivery Redesign with Focus on Value to the Patient.” The Clinical Business Intelligence Network (CBIN) is primarily focused on the upper left-hand part of the diagram, “Transparency of Cost, Quality, Risk, and Consequences.” Combined, they are two key drivers that help move organizations toward one-piece value flow.
The connection between these two networks is further illustrated in this short video clip featuring Julie Bartels, Executive Vice President, National Healthcare Information and Clinical Business Intelligence Network.
Value Must Run Across All Systems
Another way to illustrate the connection between the two networks is shown in this diagram from Jacob Raymer, President of the Institute For Enterprise Excellence: 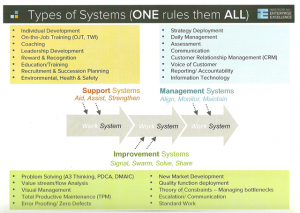
The work system (center of the diagram) in healthcare is all about patient care and the processes that directly support that care (e.g., diagnostics, testing, medication).
There are three other types of systems that support the work system:
1) Support Systems that aid, assist, and strengthen the people who work in the work system.
2) Management Systems that align, monitor, and maintain the work system.
3) Improvement Systems that help people to signal, swarm and solve problems, and share what they have learned.
Where CBI Fits
Clinical Business Intelligence is sometimes associated with “information technology” (an example of a type 2 system), but it is more than that. It is really about the flow of information through the enterprise, and the ability of the staff to interface with that information at the point of care.
There are two perspectives to be considered: 1) production, and 2) consumption. Healthcare organizations are getting better at producing analytics thanks to the myriad of software vendors who provide bolt-on reporting packages to extract analytics from the Electronic Medical Record Systems. Unfortunately, if that’s where Clinical Business Intelligence work stops, it is merely a form of very expensive waste. The real value comes from the consumption of analytics, that is, the ability of the clinical staff to see, absorb, and respond to that incoming information during the patient’s visit and make smarter decisions that benefit the patient and the enterprise as a result.
So, true and sustainable value is derived through a constant game of catchball between turning raw data into meaningful information (Clinical Business Intelligence) at the bedside, and employing standard work and patient minded delivery (lean ) at the point of care.
Making Connections: How Intelligence Feeds Improvement
In summary, we see four hypotheses about the connection between lean thinking (the primary focus of the HVN) and Clinical Business Intelligence (the primary work of the CBIN):
Hypothesis #1: Lean transformation requires focused and iterative PDSA. PDSA requires creation, collection, and on-going monitoring of meaningful (actionable) metrics in the Plan and Study phases. The tighter the feedback loop between action and measure of impact, the more frequently the PDSA process can cycle through, and the quicker the insight and improvement.
Hypothesis #2: The value achieved through application of scientific thinking and adoption of lean methods can be accelerated or negatively impacted by the scope and speed of information flow.
Hypothesis #3: Manual information collection and management is possible but prone to many forms of waste: Waiting, Underutilized Human Talent (e.g. nurse data collection), and Defects (human error). It may also limit the scope and pace of information available to support PDSA.
Hypothesis #4: Aligning lean and Clinical Business Intelligence with the mission of the enterprise and key performance indicators will accelerate and sustain performance improvements. 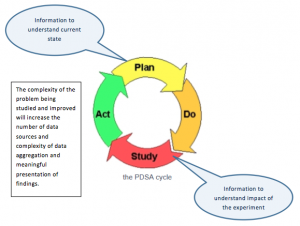 This is how we see it. How does this match your experience? Would you like to learn more and possibly participate in testing our hypotheses? If so, contact Julie Bartels, jbartels@createvalue.org, or Mike Stoecklein mstoecklein@createvalue.org to learn more.
This is how we see it. How does this match your experience? Would you like to learn more and possibly participate in testing our hypotheses? If so, contact Julie Bartels, jbartels@createvalue.org, or Mike Stoecklein mstoecklein@createvalue.org to learn more.








Leave a Reply