The Key to Breakthrough Results from Innovation: Address the Whole Care Model
Many healthcare executives are interested in building innovation capability in their organizations. Oftentimes this interest manifests as a stated objective in the enterprise strategic plan to “do innovation” and some lucky (or unlucky) soul is pulled aside and asked to add the initiative to their existing, long list of responsibilities. They end up stuck with the mandate – “go forth and innovate!”
Over the past few years, I’ve had the opportunity to speak with a number of individuals who have been put in the position of overseeing innovation. I’ve learned that what is often lacking is a clear answer to the important question—what are we innovating? Without this, it’s difficult to understand who needs to be on the team, what the innovation process looks like, and what kind of results or system impact to expect from the innovation efforts. In the absence of clear direction here, efforts tend to naturally shift towards areas that are more readily considered “innovative” by their peers. This usually means developing new devices, transforming existing equipment, programming digital interfaces for providers and patients, or incubating startups by giving them access to system resources. While these approaches can yield cool new products and experiences, their impact on the performance of the system is limited by the scope and scale of the given undertaking. The scope being defined as how many components of a given care model are being addressed by the innovation and scale meaning and how many patient lives are impacted.
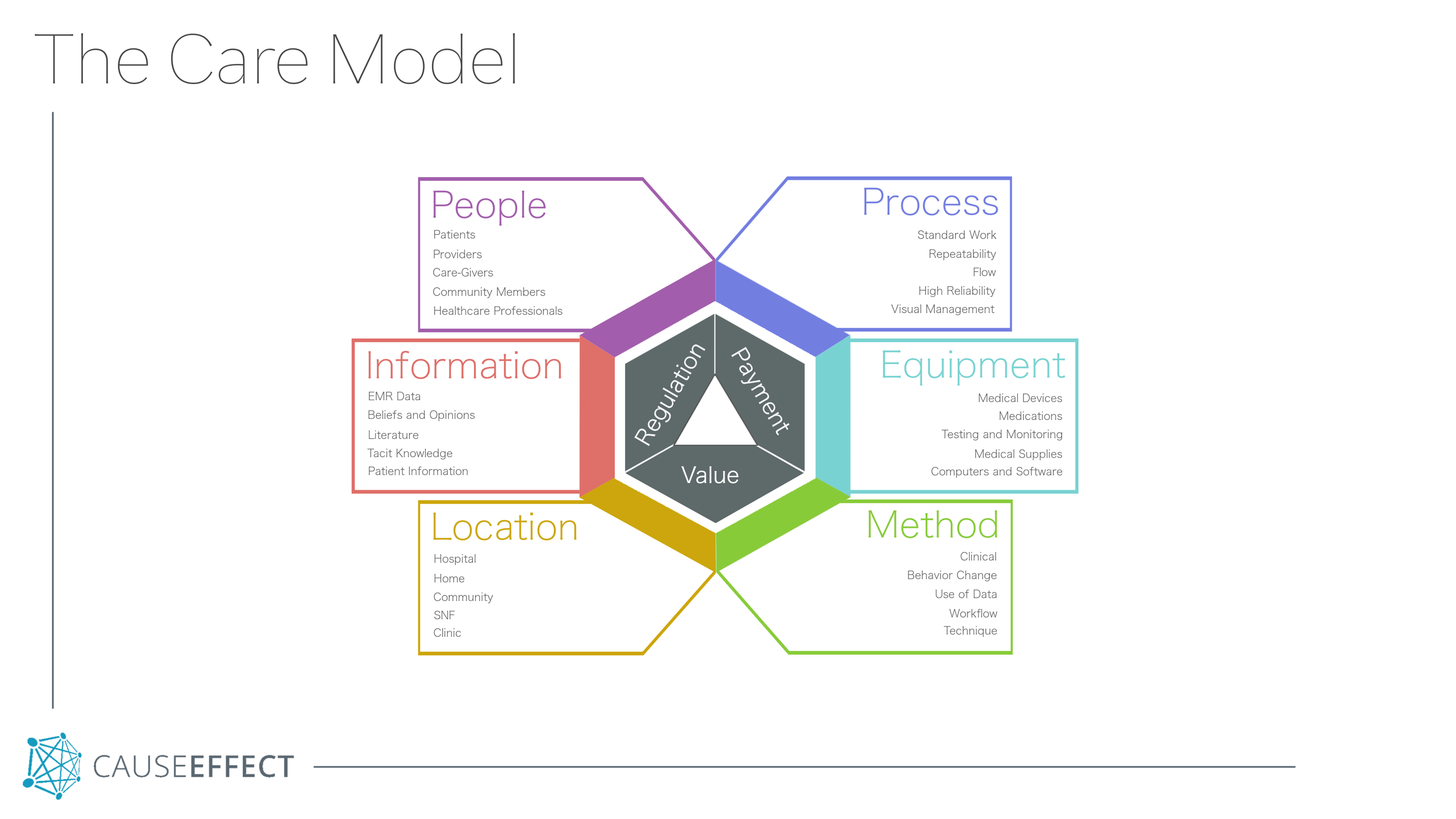
Care models are vehicles through which health systems deliver value to patients, generate revenue from payers, and adhere to regulations. They are made up of six primary components.
- People What population is being served? Who is delivering care? What level of licensure are the providers? Who are the key individuals in the patients’ lives that impact the care model?
- Process What are the core care delivery processes? What are the supporting processes? How is standard work written, maintained, and updated? How is visual management used to keep process in control?
- Equipment What medical devices and supplies are used? What software is used? What types of communication technology are utilized? What medications are used?
- Location Where is the care delivered? Where are all of the people physically? What buildings or structures are used?
- Method What clinical methods are used? How is data utilized? What best-practice techniques are taught and employed?
- Information What patient information is used in the medical record? What literature is used to support care? What is the tacit knowledge that is leveraged? How is process information used?
Care models are systems and each of the six components must work together in order to deliver meaningful results for patients and stakeholders. When innovation is focused solely on one or two components, other components of the care model will maintain existing momentum and limit the degree to which larger system impact can be realized. When innovation teams are willing to rethink four, five, or even all six of these components simultaneously, truly breakthrough system changes are possible that go far beyond what a new app or piece of equipment can do on its own.
Innovation initiatives that take on the care model as a whole need to be structured quite differently than those focused on one or two components. It must be clearly linked and prioritized within the enterprise strategic plan. Functional representation from key areas of the organization should be incorporated into the team structure. In particular, influential clinical leaders with a burning vision of a very different future need to provide leadership. Their ideas and future designs must also be balanced by a deep understanding of patient needs uncovered through ethnographic research.
Focusing innovation efforts on one or two components of a care model can be a good place to start, collect a few wins, and develop initial capability in the organization. This is the approach many systems are taking and front-line providers and staff are gaining valuable experience in human-centered design, product development, and entrepreneurial thinking. However, if the scope of projects undertaken by these teams does not expand to include additional components of the care model, meaningful changes to the overall system won’t be possible, and these teams will become increasingly frustrated. In my upcoming workshop I will be walking through important concepts and systems necessary to engage in innovation at this level. I will share first-hand experiences from care model innovation projects that impacted outcomes at a system level, and help participants think through where to start in their organizations.
Ted Toussaint, Faculty
Catalysis
Related Items
Innovation in Healthcare Workshop








Leave a Reply