Adapting Daily Management Huddles for a Hybrid Remote World

The first wave of the COVID-19 pandemic swept through New York City in March of 2020. At Mount Sinai Morningside, teams across the hospital were also in the beginning stages of implementing both communication and improvement huddles by utilizing large dry erase boards in their departments. While many frontline clinical teams were able to continue to huddle in person throughout the pandemic, many administrative and support teams shifted to working remotely.
In the summer of 2020, Mount Sinai Morningside’s executive team encouraged all departments to return to pre-COVID-19 improvement work. At that time, the Patient Care Liaison team was in their own period of change; the mostly administrative team, with new team members and new leadership, had not returned to full-time in-person work. The team had to implement daily management, complete with a board and huddle, despite the distance between them.
The Patient Care Liaison team was tasked with implementing huddles using the standard template for clinical, in-person huddles while meeting virtually. The team worked through the challenges of learning a new process and determining how to adapt the huddle standard effectively in a way that engaged every team member while they met virtually. Through hard work, coaching, and multiple iterations, they learned the value of starting small, the importance of seeing examples of what good looks like, when to hold to the standard and where they could use their creativity in adapting it, and that improvement work can continue and add value even in the midst of disruption.
Background on Implementing Daily Management at Mount Sinai Morningside
The implementation of a daily management system at Mount Sinai Morningside (MSM) began in 2019 with a pilot project to develop standards for both a daily (or per shift) communication huddle and a weekly improvement huddle. These were held in front of a large dry erase board used to visually manage the content of the huddles. Several pilot departments were selected, including two nursing departments and one ambulatory practice. Each pilot team had a member from the Lean team assigned to coach them as the department leaders worked through a PDCA of the various elements of the daily management system.
Communication huddle standards included customary topics for all departments with elements to report out, as well as open-ended questions to pull information from the team. For example, in an inpatient unit, under the topic of Flow, content might include expected admissions and discharges and an open-ended question related to anticipated challenges. By the third quarter of 2019, communication huddles had been spread to approximately 30 additional departments in the hospital.
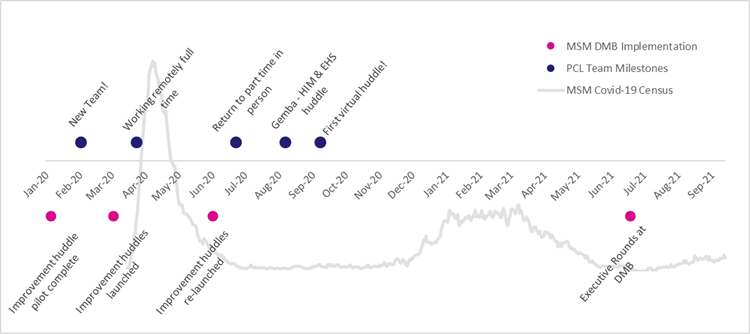
As communication huddles spread, the pilot departments continued to work with their coaches to design and iterate on the standard tools, templates, and workflows for a weekly improvement huddle. In January of 2020, preparation began to spread the improvement huddle standards to the departments already employing the communication huddle; training completed in the first weeks of March for teams who were next to adopt the improvement huddle. Due to the initial wave of the COVID-19 pandemic, the implementation of improvement huddles was immediately paused in most locations.
Communication huddles, where implemented, immediately proved their value as conditions in the hospital, policies, procedures, and staff concerns changed daily. Through the tiered huddle structure in the hospital, challenges or questions were able to escalate up from the frontline staff to the hospital and system leadership while changes and critical communications were able to flow back down to frontline teams. While improvement huddles in departments didn’t take place as designed, at the direction of the hospital incident command team, the Lean team pulled together interdisciplinary groups to use A3 thinking to work through the new challenges and workflow issues that arose daily during the first wave.
By June of 2020, the patient census at MSM had mostly returned to normal. The Lean team resumed its focus on teaching and coaching improvement huddles with refresher training for leaders and concentrated efforts coaching participating departments to find a routine. For some departments, such as the Patient Care Liaison (PCL) team, this was a fresh start. With a new leader, new coach, and workflows permanently changed by the pandemic, the team had an opportunity to leverage their creativity and find an innovative solution to define daily management in their own terms. Natalie Bergstrom, the leader of this team, shares below about the team and their experience implementing daily management.

Overview: A Unique Support Team
The Patient Care Liaison team works with inpatient providers to facilitate high quality transitions of care across inpatient and outpatient settings by coordinating post-discharge appointments. Patient Care Liaisons are an extension of the patient’s care team and participate in interdisciplinary rounds with clinical team members to effectively plan for a smooth discharge process. Interdisciplinary rounds occur daily on each inpatient unit. After rounds conclude, the PCLs visit patients at the bedside and increase health literacy by educating patients on the importance of post-acute care and procedures.
When COVID-19 arrived in New York City and Mount Sinai Health System (MSHS) instructed teams like ours to begin working from home, we had to quickly adapt our work to continue meeting the needs of our patients from a remote location. The pandemic changed the way the PCLs interacted with their patients and with one another. For example, all patient interaction was conducted by telephone once the PCLs were unable to work on the inpatient units. After a few months of working from home and once the inpatient census of COVID-positive patients had dropped substantially, our department implemented a staggered return to work plan to allow for social distancing in the office. This meant that the team was still physically separated even though hospital operations were beginning to return to normal.
With the charge to establish daily management, the PCL team set out to creatively reproduce a board and a huddle structure for this uniquely hybrid-remote team.
Our Story: Adapting the Standard for Daily Management
The Patient Care Liaison team is unlike most teams found within a hospital setting, so naturally, daily management looked different, too. The standard work for daily management and huddles at MSM was optimized for inpatient clinical teams. The dry erase board templates repeated throughout the hospital hallways did not initiate the same conversations and the content prioritized by nursing did not embody the work of the PCLs.
It was initially difficult to look beyond the board content at the overarching structure of daily management to see a framework that could be customized to fit the needs of the PCL team. As the leader, I felt paralyzed by all the decisions that had to be made to create something completely different that still fit the established mold. My improvement coach assured me that starting with something small was still a step in the right direction and she suggested that we go to the Gemba to see what ideas might spark. We went to two support services huddles together to see how other non-clinical teams had adapted the standard huddle and board.
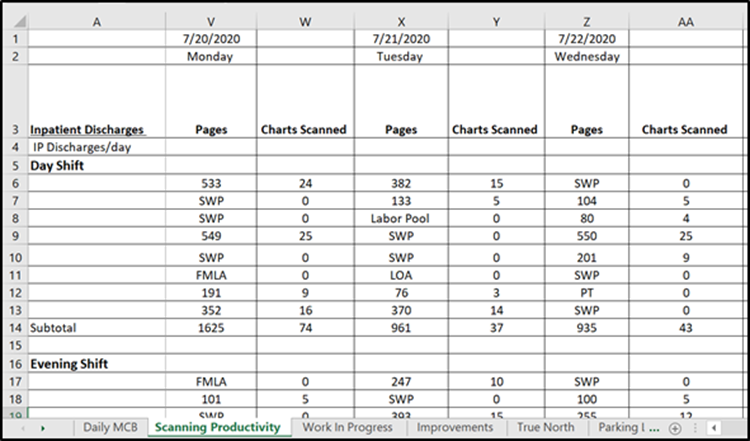
The first huddle we observed together was the Health Information Management department’s, an area that was still fully remote and conducted their huddle on Zoom. One person shared a spreadsheet for all attendees to see. Team members had prepared for the huddle by entering data into the spreadsheet to discuss. This format confirmed that a virtual huddle was as straightforward to conduct as any virtual meeting, but it demonstrated that one person had to own the content management during the huddle. My goal was to enable virtual collaboration and engagement with the daily management board (DMB) content by all team members in real-time like was characteristic of in-person huddles.
Next, we observed the Environmental Health and Safety department’s hybrid virtual huddle, watching this helped me begin to see how a team located in different places could engage around a DMB. Their department, which spans multiple hospitals, used a dry erase board that had all the visual elements of the MSM daily management template. The team at the other hospital joined the huddle virtually and viewed the board via a tablet mounted to a workstation on wheels. This still left a single person in charge of managing the board content, and I worried about my team members being able to see the board in great enough detail. I did not want network bandwidth or device type to present any engagement barriers.
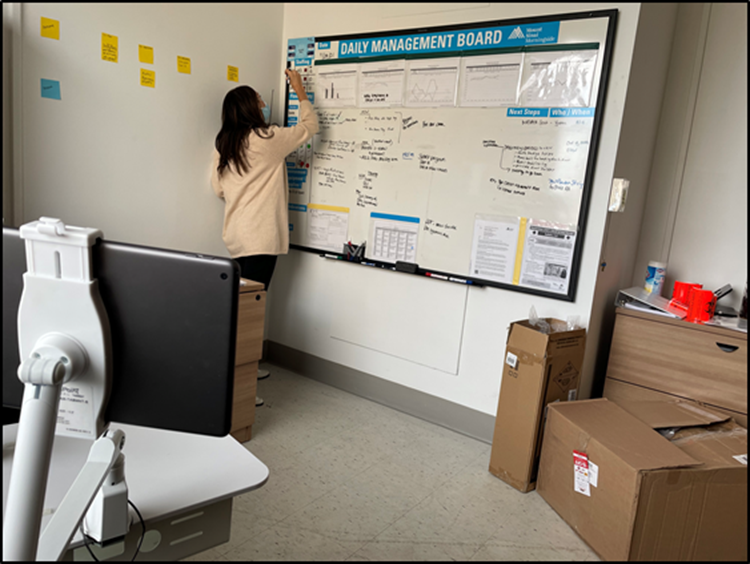
As the format began to take shape in my mind, I had to figure out what technology was best suited to our needs. Ideally, it would be something both my team and I were familiar with to minimize the learning curve. I started by studying the standard boards around the hospital and recognized that there were distinct blocks and grid-like sections for organizing information. I built our board template in Microsoft Excel since the functionality of Excel leant itself to reproducing the sections of the standard MSM daily management board in a similarly visual fashion. Excel is available on all MSHS devices, and everyone on the team had at least some familiarity with it.
When it came to content creation, I had to take a step back and look at the larger, overarching subjects guiding the huddle conversations. For example, instead of tracking the number of discharges by noon, which is a more meaningful metric for nursing, we had to ask ourselves what things impacted the flow of our daily work. The work of my team is driven by inpatient orders. The number of orders received daily serves as a lookback of workload volume, but we wanted to get ahead of the work to make sure we were adequately prepared. To predict flow, we began tracking the daily med/surg patient census. This number, combined with our staffing number for the day, would serve as the foundation of our communication huddle. When patient census is very high, color coded as a red day for the hospital, there are many patients in the Emergency Department waiting for a bed assignment. The inpatient teams will concentrate on expediting discharges of medically cleared inpatients, often resulting in an influx of orders to the PCL team. To flex to the discharge needs of the hospital, we can strip down our workflow to include less time on the inpatient units in order to spend more time at a computer working through the orders with the goal that patients have their appointments scheduled before they leave the hospital. By defining what flow was unique to our work, we figured out meaningful metrics to guide proactive planning conversations.
The next step was to figure out the modality of our huddle. MSHS had used Zoom for virtual meetings since before the start of the pandemic and had recently deployed Microsoft Teams to all Mount Sinai devices. While Zoom had the familiarity factor, I did not want one person to have to share their screen and take charge of all data management. I found that Teams allowed us to host documents that could be opened and edited by multiple users at one time, which was exactly the kind of collaboration functionality I was looking for. Each person could open the document while simultaneously using their device-integrated camera to meet virtually.
We launched our team huddles in September of 2020. It took multiple attempts for everyone to learn the technology well enough for the huddles to run smoothly, but once the team was comfortable with the format, we began iterating on the process. Each team member assigned themselves a color (green, yellow, or red) at the start of the huddle to convey how they were feeling that day. We decided that each person should assign their color as preparation for the huddle instead of picking a color during the huddle. Opening the huddle with this color visual allowed us to immediately launch into a discussion about team needs if I was seeing red or yellow. We then looked at other data points that could be pre-loaded into the DMB and where that information was sourced from. Some data is only accessible by management, but other information, like the daily med/surg patient census, was available to my team, provided they were on the hospital distribution list. Now that they receive this daily information, they are responsible for adding it to the DMB prior to our huddle.
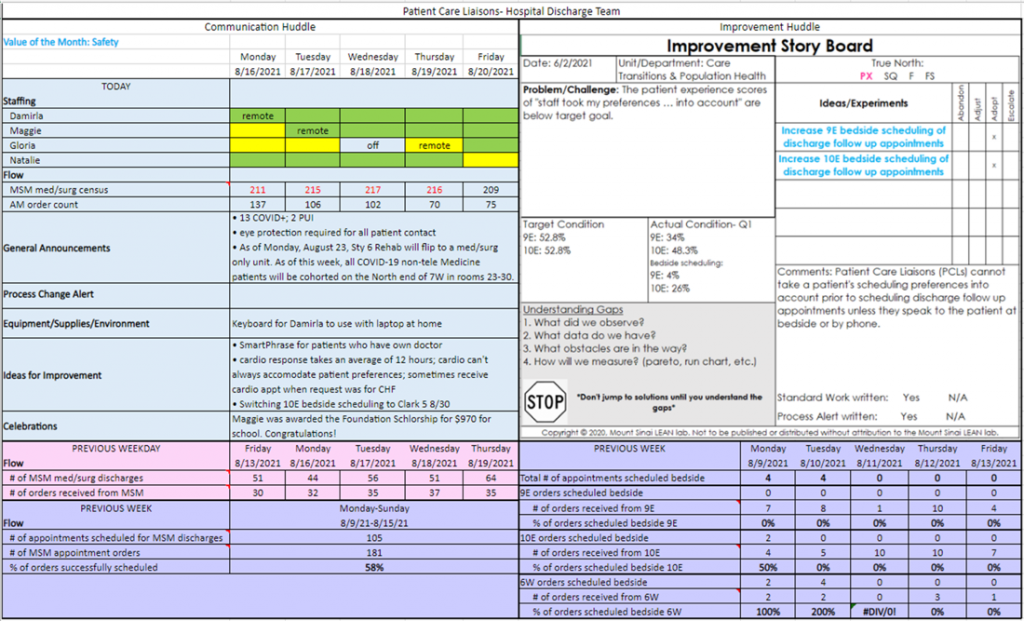
Over time we began to see trends in the types of conversations brought up during our communication huddle. The board didn’t have corresponding places to document some common topics, thus sections were added to the DMB for general announcements and parking lot items. One of the main goals of daily management is to ensure that relevant information flows in both directions from hospital leadership to frontline workers. Not all information flowing down was a process change alert, which is its own dedicated element on the board, so we created a general announcements section where we now list the daily COVID-positive patient census among other general items. We track a great number of improvement ideas on our DMB, but we have better organized ourselves by adding a parking lot section for the ideas that are not quick fixes. Finally, it became apparent that a main driver of team members’ color assignments for the day corresponded to the number of open orders in their work queue; the more orders waiting for them to complete, the more likely I saw red and yellow on the board. In the flow section of the board we added a data point for the number of open orders in the work queue each morning. Having this number handy during huddles enriches our conversation about any workflow adjustments that may be needed to sufficiently manage caseload volume.
All members of the team are responsible for preparing for the huddle by adding specific information to the DMB. As the leader, I currently facilitate the huddles, but I plan to further team development by having each member begin facilitating sections of our huddles.
Team Members’ Perspectives: Reflections from the Frontline
How do those entrenched in this work feel about daily management? Here is what we have heard from team members:
- “[Huddles] help us improve our daily execution [by] addressing problems together. We also get to observe our progress as a team every week.” – Damirla, Care Transitions Patient Care Liaison
- When asked how the current virtual board and huddle format compares to her previous experience with a physical board Maggie, Care Transitions Patient Care Liaison, explains, “They’re a little bit different now that they’re on Microsoft Teams. I can go back a couple of months because there was important information. I can check to see what my own stats were as opposed to [the physical dry erase] where once the week was done it was wiped off. I can ask a question in the Teams Chat to my manager while I’m on the floor and not have to interrupt too many things. I do work from home two days a week and I can input the information and know that everyone has access to it and it’s done in real time so if somebody changes something, I can see it immediately.”
- “It’s been quite helpful for me personally. It’s improved my performance. Us meeting on a regular basis has helped with our problems. Instead of waiting a couple of days or weeks, things will pile up. [Huddling] three times per week is really helpful. Even if you miss something, it’s always in the system where you could go back and refer to what we’ve discussed that day. In meeting with other people you get different ideas, which is really, really helpful. I think it’s the best thing for me, personally. It’s my first time with a huddle, so it’s a good idea.” – Gloria, Care Transitions Patient Care Liaison, the newest team member
Reflections and Insights from the Manager
Looking back on my team’s daily management journey, I wish we’d started sooner. Our huddles have been an excellent way to ensure short, frequent touch bases that keep all team members on the same page. We eventually figured out the customized content and format that meets our need for flexibility. We continue to make changes to our process, and we’re well positioned to do so because of the digital nature of our system.
A positive, albeit unexpected, consequence of using an online document in lieu of a dry erase board is the historical record keeping. There are countless times my team has looked back at announcements, census trends, improvement ideas, and metrics. I can reference data quicker in past weeks’ DMB versions than I can running a report out of our electronic medical record.
Launching daily management was a good lesson in starting small. I was handed a hospital standard to implement with my own team, and I struggled to see how our work and structure could fit within the expectation. As a new manager, I was also scared to deviate from what everyone else was doing. I needed the assurance from my coach that I had permission to think outside the box. While Lean methodology does encourage standard work, it isn’t rigid. Lean provides a set of tools to work smarter but is flexible enough to be applied across different teams, departments, and industries. My coach also provided (repeated) encouragement to take it one step at a time. The entire board and huddle format did not need to be clearly defined prior to beginning. She knew there would be iterations and that once we began, we would find our groove and the relevant content would reveal itself. My coach was right. When a project feels so large that it is overwhelming, I have realized the value of breaking it into smaller tasks and focusing on completing one at a time.

Reflections and Insights from the Coach
As Natalie and her team were new to huddles in general (communication and improvement), they had no pre-existing structure to fall back on when we came out of that first wave of the pandemic, and due to their need for a virtual option, they had to design something new. We often say when coaching process improvement not to let perfection be the enemy of good. Like many in healthcare, Natalie likes to do things well, so being able to imagine what a virtual huddle would look like was an important step in being able to design and implement something with her team. To help get the vision flowing, I took Natalie on a “Gemba” to a couple of other huddles that were tackling similar challenges with creative solutions.
We also spent time reviewing the intent of the various elements of the communication huddle. Recognizing that while the structure is standard, what flow or safety means to each department in planning their day is different. Brainstorming what each of those elements meant to her team in their day-to-day operations was an important step in designing what content needed to be included on their virtual template. As a coach it was important to know when to hold to the standard and where to encourage flexibility and creativity to adapt to what is meaningful to the work.
We now have about 50 teams at MSM leveraging daily management to communicate and improve in their departments. Adoption of the improvement huddles and consistency in following A3 thinking (a scientific method of problem solving, captured on a single page) as teams problem solve has been inconsistent. One pattern that has emerged is that the leaders who were most successful were either just completing, or in parallel learning, A3 thinking through the classes Lean coaches teach at MSM. The closeness of being coached through solving their own problems before moving into the role of coaching their teams to solve problems is something that the Lean coaches have learned from and are now incorporating for new leaders. Timing doesn’t always work for a new leader to take a formal class, but we have added to our onboarding standard work to coach a new leader through solving their own problem before asking them to lead it with their teams. This has also been a helpful step to include when a leader has had the training but may have had a gap in consistently practicing A3 thinking and can use that confidence boost before leading their teams.
In a fun new development, one of the departments Natalie and I initially visited is taking a page from her book. The department of Environmental Health and Safety that used a dry erase board and an iPad to “Zoom in” team members at another site is moving to a virtual board in order to make it easier for all involved to update their own information and have more hands-on involvement in the huddle.
I joined the Lean team at MSM just two weeks before our first COVID-19 patient was admitted. As that first wave took off, I saw repeatedly how the Lean culture that had been established at MSM had fostered a resilience, willingness to try new things, and iterate daily. It was obvious there was trust in the frontline teams to make suggestions, and a willingness to try, and learn from, success or failure to continue to improve. Communication huddles proved their worth immediately, as information changed rapidly. As the first wave receded, teams who needed to re-engage and regain control were empowered as they took ownership of their department and workflows through their improvement huddles. Teams like the PCLs, who implemented both communication and improvement huddles between waves, had a new method of communication established as each subsequent wave of COVID related volume came through the hospital. I am so proud of the teams who, in the face of the ongoing challenges of healthcare and the pandemic, remain committed to continuous improvement for their patients and colleagues.


Final Thoughts
We wrote this article hoping it would encourage you. The pandemic has disrupted so many routines and botched the best laid plans. It’s hard to take a step forward when we still face so much uncertainty. Working in healthcare requires great agility, perhaps now more than ever, and we hope you can use our tips to find the courage and creativity to forge ahead. Start small, identify your guardrails, and seek out examples. If today’s iteration isn’t perfect, you can always try something different tomorrow. We owe it to our patients and each other to never stop improving.







